Types of Radiation Therapy
This section provides an overview of two board categories of radiation therapy, some specific treatment types in these categories, how these treatments are delivered, and the treatment continuum in which they are used.
On this page...
External Beam Radiation Therapy
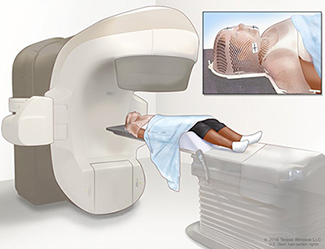
Figure 1. Radiation Therapy, External Beam (EBRT), Head And Neck.
Source: Terese Winslow (Illustrator), National Cancer Institute.
External beam radiation therapy (Teletherapy) [4] is radiation delivered from a distant source, from outside the body and directed at the patient's cancer site. External beam therapy is the radiation therapy treatment option used for most cancer patients. It is used to treat many types of tumors including cancers of the head and neck area, breast, lung, colon, and prostate.
Systems which produce different types of radiation for external beam therapy include
- cobalt-60 machines
- linear accelerators
- neutron beam machines
- orthovoltage x-ray machines
- proton beam machines
Depending upon tumor location, different levels of radiation are used for external beam therapy. Low-energy radiation does not penetrate very deeply into the body and is used mainly to treat surface tumors such as skin cancer. High-energy radiation is used to treat other deeper cancers.
Stereotactic radiation therapy involves focusing the radiation beam on a small area and delivering very high doses. The therapy targets a tumor from many different directions, so the beams of radiation converge on the tumor. This way, the ideal amount of radiation needed to destroy tumor cells is delivered directly to the tumor growth, while the amount of exposure to the area surrounding the tumor is minimized. Stereotactic radiation therapy is very effective in treating small tumors such as those in the head and brain.
Sources of external beam radiation may include, but are not limited to

Figure 2. Linear Accelerator (LINAC) that is set up to deliver stereotactic radiosurgery.
Source: Daniel Sone (Photographer), National Cancer Institute.
- betatron
- cobalt
- linear accelerator
- neutron beam
- photon beam
- proton beam
- spray radiation
- stereotactic radiosurgery such as gamma knife
- x-ray
Types of Beams
- Electrons – negative charge, beams do not travel far, limited to tumors nearer body surface
- Photons - can reach tumors deep within the body, scatter bits of radiation along path to tumor, continues to travel through normal tissue once tumor is reached
- Protons – positive charged particles, does not scatter radiation along path, stops at tumor location
Gamma Knife
Gamma knife uses a concentrated radiation dose from Cobalt-60 sources. the gamma knife is so precise that it damages and destroys the unhealthy tissue while sparing adjacent normal, healthy tissue.
Advantages of External Beam
- painless
- most patients do not require a hospital stay
- patients do not see or feel the actual treatment
- many patients can go home following each treatment
- most patients can even continue with their normal daily activities
Internal Radiation Therapy (Brachytherapy)
Brachytherapy involves placing radiation sources in the form of wires, seeds (or molds) or rods as close as possible to the tumor site. Sometimes, they may be inserted directly into the tumor. This technique is particularly effective in treating cancers of the cervix, uterus, vagina, rectum, eye, and certain head and neck cancers. It is also occasionally used to treat cancers of the breast, brain, skin, anus, esophagus, lung, bladder, and prostate.
In some instances, brachytherapy may be used in conjunction with external beam therapy. When both forms are employed, the external beam radiation is intended to destroy cancerous cells in a large area surrounding the tumor, while the brachytherapy delivers a boost, or higher dose of radiation, to help destroy the main concentrated mass of tumor cells.
There are several types of brachytherapy characterized by different methods of placing radiation inside the body including
- interstitial brachytherapy
- intracavitary brachytherapy
- intraluminal radiation therapy
- radioactively tagged molecules given intravenously
Interstitial brachytherapy involves implanting radioactive needles or wires in the tumor area. The radioactive sources may be
- may stay in the patient permanently
- put in and taken out on the same day
- removed from the body after several days
With intracavitary brachytherapy, a radiation oncologist places radioactive sources, using a metal or plastic device (applicator), in body cavities such as the vagina, uterus, or larynx to irradiate the walls of the cavity or nearby tissues. Usually the radioactive source is afterloaded into the applicator. When the specified dose of radiation has been delivered to the tumor, the physician removes the applicator containing the radioactive isotope.
Intraluminal radiation therapy delivers radiation to hollow organs. For example, a surgeon or a radiation oncologist inserts a specially designed tube or applicator into the lumen, or opening, of the esophagus to treat cancer.
Finally, radioactive particles can be attached to small molecules and given intravenously. For example, I-131 is used intravenously to treat bony metastases.

Figure 3. Radioactive Seeds.
Source: Terese Winslow (Illustrator), National Cancer Institute.
Internal therapy (brachytherapy): radioactive material sealed in needles, seeds, wires, or catheters is placed directly into or near a tumor.
The goal of radiation therapy can be curative intent or palliative. Radiation therapy is frequently used as adjuvant therapy to other treatments, most often with surgery and chemotherapy.
Radiation therapy plays a very important role in cancer treatment, using radiation to destroy cancer cells while causing minimal damage to normal cells and tissue. More than half of all cancer patients receive radiation therapy.
The decision to treat a tumor with radiation is based on the location of the primary tumor and whether the tumor cells are radiosensitive. Although radiation therapy and surgery have similar rates for eradicating some types of cancer, radiation therapy is preferred to surgery if the patient has a preexisting condition that makes surgery impossible or if surgery would require removing part or all of an organ. For example, radiation therapy may be chosen to treat cancer of the larynx in order to preserve the voice.
Radiosensitive tumors respond by promptly showing regression after moderate doses of radiation. Two examples of highly radiosensitive cancers are leukemia (cancer of the blood cells) and lymphoma (cancer of the lymphatic system).
Radiation therapy is most effective when a tumor is contained, easily accessible, and located away from major organs of the body. Testicular cancer, for example, is one of the best candidates for radiation therapy. During the process of radiation therapy for testicular cancer, the rest of the body can be easily protected from the radiation. Radiation can be directed from all angles to increase the effectiveness of the treatment.
Radiocurability means that the normal tissue-tumor relationship is such that doses of radiation to eradicate cancer can be used without excessively damaging the normal tissue. Radiocurative tumors include carcinoma of the cervix, larynx, breast, and prostate. Radiation may be the only therapy necessary for radiocurative tumors.
Generally, radiation is directed to the tumor and the immediate surrounding area. This destroys the main tumor and any nearby tumor spread. Higher total doses of radiation are needed to destroy the main tumor; lower doses are given to destroy the spread of the tumor. Because radiation affects both normal and cancerous cells, radiation therapists and physicists very carefully prescribe the radiation fields for treatment to exclude uninvolved vital organs and tissues. Patients are treated with multiple small doses of radiation with time in between treatments so their healthy cells can repair much of the radiation damage.
The physician in charge of the patient's radiation therapy is called a radiation oncologist, who develops and prescribes each cancer patient's radiation treatment plan and makes sure that every treatment is accurately given. The radiation oncologist works closely with other physicians and all members of the radiation oncology team, who are trained in the safe use of radiation, to make sure the cancer patient gets the best possible treatment.
Palliative Radiation Therapy
In addition to its curative purposes, radiation therapy may also be given to relieve pain in cancer patients. For example, radiation therapy can often relieve the pain caused by secondary bone cancer. For palliative purposes, lower radiation doses are given than for curative treatment, and usually over a shorter period of time.
Adjuvant Treatment
In order to achieve the most effective cancer curative results, radiation treatment is frequently used as adjuvant therapy to other treatments. Radiation treatment may be administered (neoadjuvant) before or (adjuvant) after surgical treatment. Sometimes, surgery may effectively remove the gross tumor, but there may be a limit to the amount of adjacent tissue that can be removed without impairing function. Post-surgery radiation treatment can be administered to destroy microscopic residual cancer cells left after surgery. Sometimes, pre-surgery radiation treatment is administered to shrink the tumor so that it can be surgically removed more easily or make the operation less invasive, thereby preserving more normal tissue. Based on studies, better cancer treatment outcomes result after the combination of radiation therapy and/or chemotherapy after surgery.
To ensure the success of radiation treatment, the radiation oncologist tailors each patient's treatment to make sure it is safe and effective. A careful treatment plan is often made, and then practiced using a simulator before any actual treatment begins.
There are many data item fields that must be entered into the registry abstract related to radiation therapy, these include
- Date Radiation Started
- Location of Radiation Treatment
- Phase I Radiation Primary Treatment Volume
- Phase I Radiation Draining Lymph Nodes
- Phase I Radiation Treatment Modality
- Phase I External Beam Planning Tech
- Phase I Dose per Fraction
- Phase I Number of Fractions
- Phase I Total Dose
The same above listed data items are captured for Phase II, and Phase III radiation therapy. Phase II radiation was previously called the “boost”. Specific instructions for coding these data items can be found in the Commission on Cancer (CoC) STORE (Standards for Oncology Registry Entry). There is also a guide titled “CTR Guide to Coding Radiation Therapy Treatment in the STORE
” available on the CoC website. It provides specific guidance to code specific radiation treatment modalities, abbreviations and other helpful information related to coding the radiation treatment data items.
Updated: December 21, 2023
Suggested Citation
SEER Training Modules: Types of Radiation Therapy. U.S. National Institutes of Health, National Cancer Institute. Cited 11 February 2026. Available from: https://training.seer.cancer.gov.